Specialities
- Home
- Perianal or Anal Fistula Treatment
- Home
- Perianal or Anal Fistula Treatment
What is Perianal or Anal fistula?
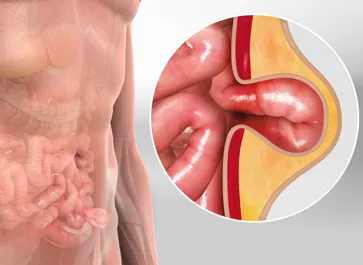
A Perianal or Anal Fistula is an abnormal connection or tract that forms between the anal canal and the skin surrounding the anus. This passage, often lined with infected tissue, can cause persistent drainage, pain, and discomfort.
A Perianal or Anal Fistula is a pathological condition characterised by an abnormal tract or tunnel that forms in the tissue around the anus. This condition typically arises as a result of infection or inflammation in the anal glands, leading to the development of a tunnel-like passage that connects the anal canal to the skin near the anus. Perianal fistulas are often associated with various anorectal disorders, with the most common being Crohn's disease.
What are the causes of Perianal or Anal fistula?
Perianal or Anal fistula are often the result of infection or inflammation in the anal glands, leading to the formation of abnormal tracts or tunnels. The causes of Perianal or Anal Fistulas can vary, and in some cases, the exact cause may not be easily identified. Here are common causes and contributing factors:
- Inflammatory Bowel Disease (IBD):
- Crohn's Disease:One of the most significant contributors to Perianal or Anal Fistulas is Crohn's disease, which is a type of inflammatory bowel disease. In Crohn's disease, inflammation can occur anywhere in the digestive tract, including the anus and rectum, leading to the formation of fistulas.
- Infection:
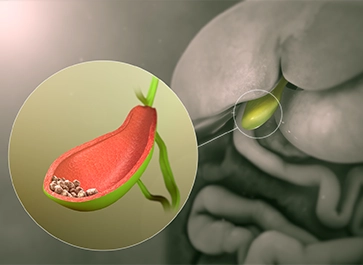
- Anal Gland Infection:Infections of the anal glands, which are small glands located just inside the anus, can result in the development of Perianal or Anal Fistulas. These infections may occur spontaneously or as a complication of conditions like anal abscesses.
- Abscess Formation:
- Perianal Abscess:If an anal abscess (a collection of pus) is not adequately treated or drained, it may lead to the development of a Perianal or Anal Fistula as the infection seeks an outlet for drainage.
- Trauma:
- Anal Trauma:Injury or trauma to the anal region, such as during childbirth or other accidents, can sometimes contribute to the formation of Perianal or Anal Fistulas.
- Cryptoglandular Infections:
- Bacterial Infections:Bacterial infections in the anal glands, commonly caused by bacteria such as Staphylococcus or Escherichia coli, can lead to inflammation and the subsequent development of fistulas.
- Sexually Transmitted Infections (STIs): Certain sexually transmitted infections, such as syphilis or herpes, can contribute to the development of Perianal or Anal Fistulas.
What are the Symptoms of Perianal or Anal fistula?
If you suspect you have a Perianal or Anal Fistula or are experiencing symptoms associated with this condition, it is important to seek medical advice promptly. Here are some signs and situations that warrant contacting a healthcare professional:
- Anal Pain: Persistent or recurrent pain around the anus is a common symptom of Perianal or Anal Fistulas. The pain may be throbbing, aching, or sharp in nature.
- Discharge: Continuous or intermittent drainage of pus, blood, or other fluids from an opening near the anus is a characteristic symptom. The discharge may have a foul odour.
- Swelling and Redness: Swelling and redness around the anal region may be present, especially near the site of the fistula opening. This can contribute to discomfort and pain.
- Itching or Irritation: Itching or irritation around the anus may occur, often due to the drainage and inflammation associated with the fistula.
- Skin Changes: Changes in the skin around the anus, such as the development of a lump or skin tag, may be observed.
- Recurrence of Abscesses: Individuals with Perianal or Anal Fistulas may experience recurrent abscesses in the anal or perianal area. These abscesses can be painful and may require drainage.
- Painful Bowel Movements: Pain or discomfort during bowel movements is common, particularly if the fistula is located close to the anal canal.
- Fever and Systemic Symptoms: In cases where the fistula is associated with infection, individuals may experience fever, chills, and other systemic symptoms. This indicates a more severe condition that requires prompt medical attention.
- Changes in Bowel Habits: Some individuals may experience changes in bowel habits, such as diarrhea or constipation, especially if the Perianal or Anal Fistula is associated with an underlying inflammatory bowel disease like Crohn's disease.
Diagnosis for Perianal or Anal fistula
Diagnosing a Perianal or Anal Fistula typically involves a combination of medical history review, physical examination, and diagnostic tests. The process is usually carried out by a healthcare professional, such as a gastroenterologist or colorectal surgeon. Here are the key components of the diagnostic process for Perianal or Anal Fistulas:
- Medical History: The healthcare provider will inquire about your medical history, including any symptoms you are experiencing, their duration, and any relevant factors such as a history of inflammatory bowel disease (IBD), prior anal abscesses, or other relevant conditions.
- Physical Examination:A thorough physical examination is crucial for identifying the presence and characteristics of a Perianal or Anal Fistula. The healthcare provider will visually inspect the perianal region, looking for signs of swelling, redness, discharge, and other abnormalities.
- Imaging Studies:Various imaging studies may be used to visualize the anatomy of the perianal region and identify the fistula tract. Common imaging modalities include:
- Magnetic Resonance Imaging (MRI):MRI is often the preferred imaging method for evaluating Perianal or Anal Fistulas. It provides detailed images of soft tissues and can help determine the location, extent, and complexity of the fistula.
- Ultrasound: Transrectal or transperineal ultrasound may be used to assess the perianal region and identify fistula tracts.
- Fistulogram: In some cases, a fistulogram, which involves injecting contrast material into the fistula tract, may be performed to obtain X-ray images.
- Endoscopic Evaluation: In certain situations, endoscopic procedures such as flexible sigmoidoscopy or colonoscopy may be recommended to assess the rectum and colon. This is particularly relevant if an underlying condition, such as Crohn's disease, is suspected.
- Laboratory Tests: Blood tests may be conducted to check for signs of infection or inflammation, as well as to assess general health. In cases associated with inflammatory bowel disease, specific blood markers may be measured.
Treatments for Perianal or Anal fistula
The treatment of Perianal or Anal Fistulas is individualized based on factors such as the characteristics of the fistula, its location, the underlying cause, and the overall health of the patient. Treatment may involve a combination of medical and surgical interventions. Here are common approaches to treating Perianal or Anal Fistulas:
- Fistulotomy:
- Fistulotomy involves making an incision along the entire length of the fistula tract to create an open channel. This allows for drainage and promotes healing.
- Indications: Suitable for simple or low intersphincteric fistulas without significant branching.
- Considerations: Fistulotomy may lead to faster healing but is not always appropriate for complex or high intersphincteric fistulas due to the risk of incontinence.
- Seton Placement:
- A seton is a thread or tube that is placed through the fistula tract to promote drainage and prevent abscess formation. There are two types: cutting setons, which gradually cut through the fistula, and non-cutting setons, which are left in place to maintain drainage.
- Indications: Commonly used for complex or high intersphincteric fistulas.
- Considerations: Seton placement is often a staged procedure, and multiple set changes may be required for complete healing.
- Fistulectomy:
- Fistulectomy involves the surgical removal of the entire fistula tract.
- Indications: Suitable for cases where the fistula tract can be easily excised without causing damage to surrounding structures.
- Considerations: Appropriate for certain simple or low intersphincteric fistulas.
- Advancement Flap Repair:
- This procedure involves using nearby healthy tissue to create a flap that covers the internal opening of the fistula, promoting healing.
- Indications: Often used for more complex fistulas, especially those associated with a high risk of incontinence after fistulotomy.
- Considerations: The procedure may require multiple stages, and careful patient selection is crucial.
- Ligation of Intersphincteric Fistula Tract (LIFT):
- The LIFT procedure involves placing sutures to close the internal opening of the fistula, promoting healing.
- Indications: Suitable for transsphincteric fistulas.
- Considerations: LIFT is a technique aimed at reducing the risk of incontinence associated with traditional surgical approaches.
- Fibrin Glue Injection:
- Fibrin glue is injected into the fistula tract to seal it. This procedure is less invasive than some other surgical options.
- Indications: May be considered for specific types of fistulas, but its effectiveness can vary.
- Considerations: Success rates may be lower compared to more traditional surgical approaches.
- Placement of Plugs or Flaps:
- Synthetic plugs or biological flaps may be used to close the internal opening of the fistula.
- Indications: Considered for certain types of fistulas
- Considerations: The success of plug or flap procedures can vary, and careful patient selection is important.
Lifestyle changes after Perianal or Anal fistula
After undergoing treatment for a Perianal or Anal Fistula, certain lifestyle changes may be recommended to promote healing, prevent recurrence, and improve overall well-being. It's important to note that these suggestions may vary based on individual circumstances, the severity of the condition, and any underlying causes such as Crohn's disease. Here are some general lifestyle changes that individuals with a history of Perianal or Anal Fistula may consider:
- Maintain Good Anal Hygiene: Keep the anal area clean by gently washing with warm water after bowel movements. Avoid harsh soaps and use mild, unscented cleansers. Use soft, moistened toilet paper or wipes to avoid irritation and friction during cleansing.
- Avoid Straining During Bowel Movements: Straining during bowel movements can exacerbate anal issues. Ensure an adequate fiber intake, drink plenty of water, and consider stool softeners if needed to prevent constipation and reduce the need for straining.
- Healthy Diet: Adopt a well-balanced and nutritious diet rich in fruits, vegetables, whole grains, and lean proteins. A healthy diet supports overall digestive health.
- Regular Exercise: Engage in regular physical activity, as exercise can help promote bowel regularity and overall well-being. Consult with healthcare providers before starting any new exercise regimen.
- Avoid Prolonged Sitting: Prolonged sitting can put pressure on the perianal area. If possible, take breaks and stand or walk periodically.
- Quit Smoking: If applicable, quitting smoking is beneficial for overall health and may reduce the risk of complications and recurrence. Smoking is a known risk factor for inflammatory bowel disease, which is associated with Perianal or Anal Fistulas.
- Manage Stress: Stress management techniques, such as mindfulness, meditation, or yoga, may help reduce stress levels. Stress can potentially exacerbate symptoms in certain individuals.
- Regular Follow-up Appointments: Attend regular follow-up appointments with healthcare providers to monitor progress, discuss any ongoing symptoms, and adjust treatment plans if necessary.
- Be Mindful of Sexual Health: Individuals with Perianal or Anal Fistulas should communicate with their healthcare providers about any concerns related to sexual health. In some cases, it may be advisable to avoid certain sexual activities during the healing process.
Frequently Asked Questions:
1. What is a Perianal or Anal Fistula?
A Perianal or Anal Fistula is an abnormal tunnel or tract that forms between the anal canal and the skin near the anus. It is often associated with infection or inflammation in the anal glands.
2. What causes Perianal or Anal Fistulas?
Common causes include inflammatory bowel disease (especially Crohn's disease), anal gland infections, abscesses, trauma, and certain infections.
3. What are the symptoms of Perianal or Anal Fistulas?
Symptoms include anal pain, drainage of pus or blood, swelling, redness around the anus, itching, and recurrent abscesses.
4. How are Perianal or Anal Fistulas diagnosed?
Diagnosis involves a combination of medical history review, physical examination, imaging studies (such as MRI or ultrasound), and sometimes endoscopic evaluation.
5. What are the treatment options for Perianal or Anal Fistulas?
Treatment may include antibiotics, immunosuppressive medications, drainage of abscesses, seton placement, fistulotomy, advancement flap repair, and other surgical interventions.
6. Can Perianal or Anal Fistulas be treated without surgery?
In some cases, medications and lifestyle changes may manage symptoms, but surgery is often necessary for definitive treatment.
7. Is Perianal or Anal Fistula surgery risky?
The risk depends on the type of surgery and the characteristics of the fistula. Potential risks include infection, bleeding, and, in some cases, incontinence.
8. How long does it take to recover from Perianal or Anal Fistula surgery?
Recovery time varies based on the type of surgery and individual factors. Some procedures may require weeks to months for full recovery.
9. Can Perianal or Anal Fistulas come back after treatment?
Recurrence is possible, especially if underlying conditions like Crohn's disease are present. Regular follow-ups are crucial for monitoring and managing recurrence.
10. Are there lifestyle changes after Perianal or Anal Fistula treatment?
Yes, maintaining good anal hygiene, a healthy diet, avoiding straining during bowel movements, and other lifestyle changes may be recommended to promote healing and prevent recurrence.